[ad_1]
By Marie-Louise Connolly, BBC News NI health correspondent
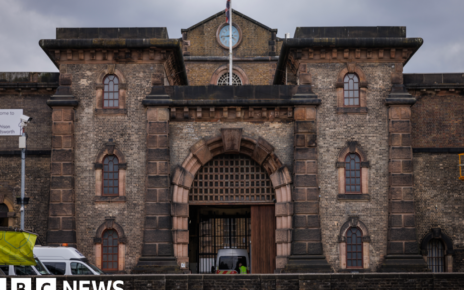
 Getty Images
Getty ImagesHealthcare staff who deliberately withhold information should face criminal prosecution in cases involving patient safety and deaths, according to Northern Ireland’s human rights commissioner.
In her first public interview on duty of candour, Alyson Kilpatrick told BBC News NI there was an obligation on doctors to be fully truthful in order to protect lives.
A duty of candour is an onus on staff to be open and transparent with patients and families when mistakes are made in a patient’s care.
However, the British Medical Association (BMA) does not agree that criminal sanctions should be linked with a duty of candour, and has said it would go against creating a culture of openness and transparency.

Alan Roberts, whose daughter’s death was examined by the Northern Ireland hyponatraemia inquiry which found there had been a “cover-up” into how she died, said doctors must be legally bound to tell the truth.
Claire Roberts was one of five children whose deaths at hospitals in Northern Ireland were examined by the 14-year-long inquiry. It was heavily critical of a health service it deemed to be “self-regulating and unmonitored”.
Mr Roberts said “the public will be shocked to find there is no legal binding duty on a doctor to tell a patient when there have been failures or when they’ve been at fault”.
“It’s a very defensive and toxic system. It’s totally frustrating for us, we’ve been through enough, we lost our daughter, and we are having to fight for some sort of change within our health system and it’s not progressing,” he said.
“Why spend the money on a public inquiry if we aren’t going to learn the lessons from that public inquiry?”
Mr Roberts said the Department of Health had been “dragging its feet” in implementing a duty of candour.
He said an honest doctor had “nothing to fear from being open and honest with their patients”.
‘Close ranks during scandals’
Health Minister Mike Nesbitt said the question was how to create a “regime that minimises the chill factor that deters individuals from being candid, and maximises willingness and responsibility to engage in an honest review of what went wrong”.
“I wish to assess the impact defined sanctions is likely of have on that balance,” he said.
The recently published Infected Blood Inquiry report coupled with the ongoing evidence at the Horizon Post Office Inquiry have ignited debate about the principle of candour and why institutions including the health and civil service appear to close ranks during scandals.
While there is a professional and moral duty on staff to do that, several public inquiries have found significant failings where information was deliberately withheld.
However, the BMA said the concept was unworkable and the Department of Health in Northern Ireland got it wrong when it linked sanctions with duty of candour in the same sentence in its 2021 consultation.
Dr Alan Stout, who represents the doctors’ union in Northern Ireland, said there should be criminal sanction if there is criminal activity, but linking it inextricably with a duty of candour threatened how doctors carried out their normal jobs.
“It hasn’t worked because the initial plans were all wrong and that was linking that complete sentence of duty of candour with criminal sanction,” said Dr Stout.
“It will never work, and we will go backwards rapidly if we continue with that full sentence. But if we work together with an individual duty of candour and an organisational duty of candour, we can absolutely make it work.”
The infected blood inquiry chair, Sir Brian Langstaff, has called for a statutory duty of candour to be imposed on civil servants as well as healthcare leaders in the wake of his findings.
The first recommendation, which Justice O’Hara listed in his 2018 hyponatraemia report, was for a statutory duty of candour to be enacted in Northern Ireland – to put a legal requirement of honesty on those working in the healthcare system.
The senior judge said this should apply where “death or serious harm has been or may have been caused to a patient” and that “criminal liability should attach to breach of this duty”.
However, both the BMA and the General Medical Council (GMC) oppose this.

The human rights commissioner said there had to be a criminal sanction when something significant had gone wrong that could lead to death or serious harm.
“Up until now a duty of candour has been a moral obligation and there’s been no sanction attached to it,” said Alyson Kilpatrick.
“I know there are disciplinary codes that require you (staff) to be open and honest with the patient, but who knows what that means. This is turning what is the right thing to do into the legal thing to do.
“We have numerous inquiries, but nothing has changed in practice or in the law that’s made a difference. So if it keeps happening, if these things keep happening over decades, you’ve got to change something, something has got to give.
“I do wonder why there seems to be something emotive about attaching the word criminal to it (duty of candour).
“It is unlikely people are going to end up in prison – but if somebody has deliberately failed to notify a serious adverse incident resulting in death, maybe that has to be a sanction that is available – it is a very, very serious failure.”
[ad_2]
Source link freeslots dinogame telegram营销