[ad_1]
 Glody Murhabazi
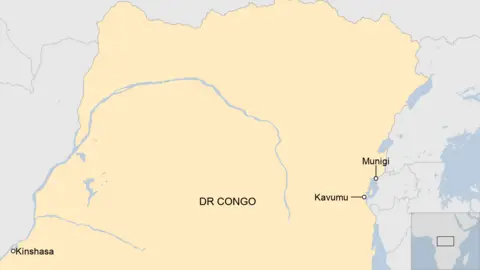
Glody MurhabaziWith mpox being declared a public health emergency of international concern by the World Health Organization because of its rapid spread, all eyes have been on the Democratic Republic of Congo, which accounts for nearly all of this year’s recorded cases and more than 450 deaths.
In visits to treatment centres in the east of the country, the BBC has found children are worst affected by the illness, which can be deadly.
“It began like a small, inflamed spot. The mother squeezed it and watery discharge came out. Then another developed, and after a short period, they were all over the body,” says Alain Matabaro, describing how mpox developed in his six-year-old son Amani.
He started recovering after four days of treatment at a clinic in Munigi, close to the major eastern Congolese city of Goma.
Some 75% of the cases being seen by medics there are under the age of 10, according to Dr Pierre-Olivier Ngadjole who works for the charity Medair.
Young people seem to be particularly badly affected by the mpox outbreak because of their less developed immune systems.
Dr Ngadjole also blames overcrowding at a nearby camp set up for people forced from their homes by conflict in the region. One way mpox is spread is through very close contact and children “are always playing together. They don’t really care about social distance,” he tells the BBC.
“You can also see in the households, they even spend the night in the same bed. You can find three, four, five children. The transmission is present on a daily basis.”
Since June, the clinic in Munigi, which provides free treatment including antibiotics to treat skin infections, paracetamol and safe drinking water, has dealt with 310 mpox cases. It is now seeing between five and 10 new admissions each day.
No-one has died from the disease there and Dr Ngadjole believes it is because people are seeking help early.
“I think it’s very important to provide free health services especially in this context… [It] means people don’t face any financial barrier, they come early to the health facility.”
It is a different story 80km (50 miles) south-west of Munigi, on the other side of Lake Kivu, at a hospital in Kavumu.
Eight-hundred patients have been seen there since June and eight have died – all under the age of five.
 Glody Murhabazi
Glody MurhabaziTwo-year-old Ansima Kanigo caught mpox from one of her four siblings, who have all had the disease.
Her mother, Nzigire Kanigo, 35, had no idea what it was at first.
“This is the first time I’ve seen it. When my child got sick, the other parents told me it might be measles, but we started treating measles and failed, so we decided to come here.
“God bless the doctor who has brought the drugs… Three [children] are cured – they are at home. I only have two who I am admitted with now in this hospital. I thank God.”
The medical director at the hospital, Dr Robert Musole, says the outbreak should not be underestimated by the authorities.
“The situation is really serious, and we’re so overwhelmed, because we have a small capacity, but we’re in great demand.
“The first challenge we face in this response is the accommodation of patients. The second challenge is the availability of medicines, which we don’t have.”
Across eastern DR Congo, there are several camps for the millions who have fled their homes as various rebel groups operate in the area.
People are often crammed into makeshift structures and living in poor conditions without good sanitation – the perfect place for mpox to run rampant.
Health workers have been visiting places like Mudja camp near Mount Nyiragongo, to educate people on what to do when they spot symptoms, such as limiting contact with others.
“This disease has brought us a lot of fear that we shall all get sick,” says Josephine Sirangunza, who lives in the camp with her five children.
She says the government needs to give out some basic equipment to help stop the disease spreading.
“When we see someone getting sick, we worry about how to protect ourselves.”
It is a sentiment shared by Bosco Sebuke, 52, who has 10 children.
“We have been sensitised [about mpox], but we are full of fear because we are crowded in our shelters. We sleep in very poor conditions, we share bedding, so prevention is difficult and because of that, we are afraid,” he says.
The outbreak in eastern DR Congo is of a new strain of mpox called Clade 1b and it has now spread to neighbouring countries.
Last week, the Congolese government said it hoped that vaccines would start to arrive from the US and Japan soon. Until then, the country does not have any vaccines despite being at the epicentre of the virus.
Mr Matabaro, the father of Amani who is now recovering from mpox, says he is hopeful with news that vaccines could be on their way.
But the distribution will be extremely limited and, as Dr Ngadjole says, vaccination is just one aspect of reducing the spread of the virus.
“The [easiest] action to put in place is to improve the hygiene. When we improve the hygiene at household level, when we improve the hygiene at community level, it’s very easy to decrease the risk of transmission.”
Ms Sirangunza echoes the doctor’s thoughts: “Tell our leaders to send us medicine, soap, and other protective measures so that we don’t get infected.”
 Getty Images/BBC
Getty Images/BBC[ad_2]
Source link freeslots dinogame telegram营销