[ad_1]
 Getty
GettyThe government has suggested weight-loss drugs could boost the economy by helping obese people in England get back to work.
But NHS experts have warned treatment services are already overstretched trying to deal with unprecedented demand from patients wanting these drugs.
How do Wegovy and Mounjaro work and how successful are they?
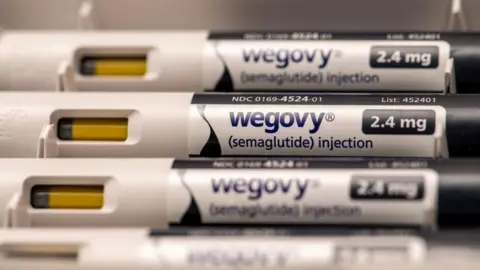
There are two drugs on the market – semaglutide, marketed under the brand name Wegovy, and tirzepatide, sold as Mounjaro. Semaglutide is also used in the diabetes treatment Ozempic.
Both Wegovy and Mounjaro are given as weekly injections via pre-filled pens that can be self-administered into the upper arm, thigh or stomach.
They work as an appetite suppressant by mimicking a hormone called glucagon-like peptide-1 (GLP-1).
This intestinal hormone is released after eating, and typically makes people feel fuller.
Mounjaro also affects another hormone, glucose-dependent insulinotropic polypeptide (GIP), which affects metabolism and helps regulate energy balance.
Patients typically start on a low dose which is gradually increased until they reach a higher maintenance dose.
People taking these drugs typically start to lose weight within a few weeks.
Clinical trials suggest that – when combined with changes to their diet, exercise and behavioural support – Wegovy users could lose more than 10% of their body weight after a year on the treatment.
Other trials suggest Mounjaro users might lose even more. But it is difficult to compare the two treatments and crucially, user of either can put weight back on once they stop treatment.
Who can get weight-loss drugs on the NHS?
At the moment, only Wegovy is available on the NHS in England, Wales and Scotland, but Mounjaro will soon be offered too.
Wegovy can only be prescribed by specialist weight management services and access to these is restricted.
To qualify, adults must have at least one pre-existing weight-related health condition such as high blood pressure and be obese.
People with cardiovascular disease and who are classed as overweight, but not quite obese, can also be given the drug.
Patients should follow a diet and physical activity programme, and the drug should be only prescribed for a maximum of two years, according to NHS guidelines.
 Getty Images
Getty ImagesThere have been reports of Wegovy shortages, although the manufacturer Novo Nordisk says the NHS has a protected supply.
Prime Minister Sir Keir Starmer told the BBC that government proposals to give weight loss jabs to unemployed people in England living with obesity could be “very important” for the economy and individuals’ health.
But weight-loss specialists have warned that NHS obesity services are already struggling to deal with demand for these drugs, and that the injections should only be used as part of a wider treatment plan.
Are weight-loss drugs available privately and what do they cost?
Both drugs can be bought privately, including at some supermarkets, chemists and high-street clinics.
Pens typically cost between £200 and £300, depending on the dose.
The drugs should not be bought from non-regulated sources.
A BBC investigation in November 2023 found online sellers offering semaglutide as a medicine, without a prescription.
It also found the drug being offered in beauty salons in Manchester and Liverpool.
What are the side-effects of weight-loss injections?
The most common side-effects are feeling sick, vomiting, bloating, constipation and diarrhoea. Some people report hair loss.
For many the side-effects are manageable and tend to go away in time; others say they stopped taking the drugs because of them.
In rare cases, serious side-effects can include gallbladder and kidney problems and depression.
Experts warn the complications can be worse if the drugs are abused, for example, taken as a quick fix to lose a few pounds or bought from unregulated online sellers.
Doctors say they have seen dangerous, life-threatening complications such as inflammation of the pancreas in such cases.
That is why experts say they should only be used under medical supervision.
What happens when you stop taking weight-loss drugs?
There is always the risk that someone will put on weight again as stopping treatment means their normal food cravings return.
That is why experts recommend that people make changes to their diet and exercise regime while on the treatment to try to make sure the healthy habits are retained.
Health Secretary Wes Streeting has warned about the danger of people developing a “dependency culture” on these drugs.
And the research suggests people do put most of the weight back on within a year of stopping.
 Getty Images
Getty ImagesWhat is a healthy BMI and what is obesity?
The term obese describes a person who has excess body fat.
In the UK it’s estimated that around one in every four adults is obese.
The standard way of categorising people’s weight is by calculating their body mass index, or BMI, which means dividing an adult’s weight in kilograms by the square of their height in metres.
For most adults, if your BMI is:
- below 18.5 – you’re in the underweight range
- 18.5 to 24.9 – you’re in the healthy weight range
- 25 to 29.9 – you’re in the overweight range
- 30 to 39.9 – you’re in the obese range
- 40 or above – you’re in the severely obese range
Those with an Asian, Chinese, Middle Eastern, Black African or African-Caribbean family background need to use a lower BMI score to measure overweight and obesity:
- 23 to 27.4 – overweight
- 27.5 or above – obese
BMI has some limitations because it measures whether a person is carrying too much weight but not too much fat.
For example, people who are very muscular can have a high BMI without much fat.
But for most people, it is a useful indication of whether they are a healthy weight.
[ad_2]
Source link




